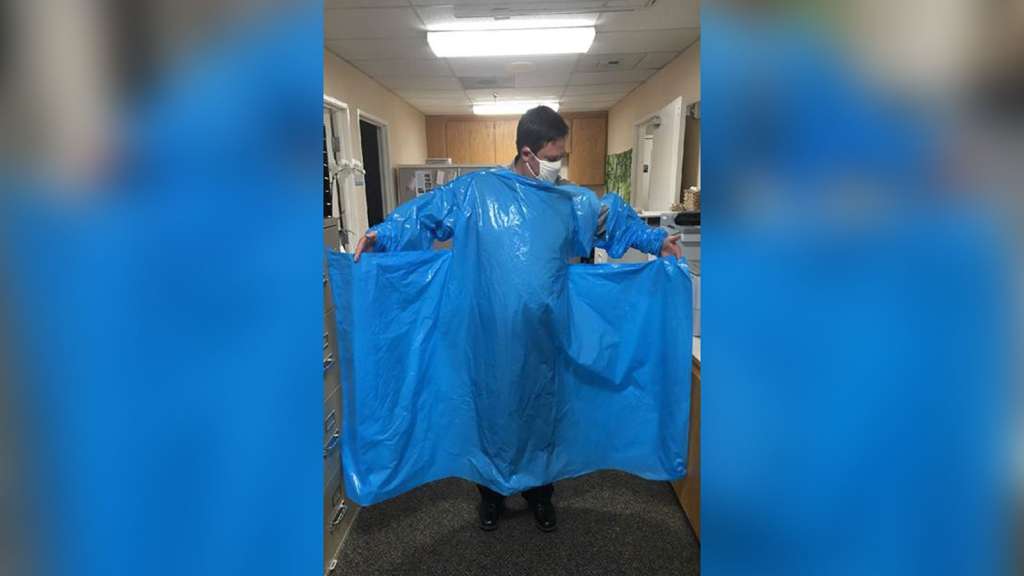
(CNN) — Nursing homes with urgent needs for personal protective equipment say they’re getting gowns that look more like large tarps — with no holes for hands — and surgical masks that are paper-thin as part of the administration’s initiative to bolster supplies for vulnerable populations amid the pandemic.
“It would be funny if the stakes weren’t so high,” a Washington state official told CNN.
In late April, President Donald Trump announced an effort to shore up supplies to nursing homes, whose residents and staff have been among those most at risk of Covid-19. The Federal Emergency Management Agency was at the helm of the effort to send additional shipments to nursing homes.
For weeks, nursing home associations have tried to call attention to the elderly population and the lack of supplies to properly care for them.
“Too often, the only signs of FEMA’s much-hyped promise of PPE shipments—an allotment of gowns, gloves, masks and goggles based on staffing size of the provider—are scattershot delivery with varying amounts of rag-tag supplies,” said Katie Smith Sloan, president and CEO of LeadingAge, an association of nonprofit providers of aging services, in a statement.
“As FEMA’s own deadline for shipment approaches, many nursing homes still don’t know if and when they’re going to receive anything,” she added. Sloan was among the attendees at the event where Trump initially announced the FEMA shipments.
In a statement to CNN, FEMA said that all personal protective equipment delivered by the agency “meets FDA or AAMI (Association for the Advancement of Medical Instrumentation) certification,” but conceded concerns had been raised.
“The AAMI-approved gowns came with instructions from the manufacturers. However, due to concerns from those who received them, the contractor is working on a short instructional video about proper use of these gowns which will be shared with the nursing homes,” a FEMA spokesperson said in a statement.
Nearly 26,000 nursing home residents have died from coronavirus, according to a recently released report. One quarter of nursing homes had at least one case, and one in five had at least one death, according to the Centers for Medicare and Medicaid Services. The cases were more prevalent in poorly rated facilities, which typically have weaker infection controls and fewer staffers per resident.
FEMA, under the direction of the White House coronavirus task force, coordinated two shipments totaling a two-week supply of personal protective equipment to nearly 15,000 nursing homes across the country, according to the agency.
FEMA said each nursing home would receive two separate shipments — one starting in May and another beginning in June. Combined, the agency estimated the personal protective equipment included more than 11.7 million surgical masks, nearly 53.3 million gloves, more than 1.2 million goggles and other eye protection, and nearly 12.9 million gowns.As of June 9, 13,654 PPE packages had been shipped to nursing homes in all 50 states, Guam, Puerto Rico and the District of Columbia, the FEMA spokesperson said, adding that since the initial deliveries, the agency has added more allotments.
A spokesperson for Genesis HealthCare, one of the largest nursing home chains in the United States, said FEMA sent defective isolation gowns to two nursing home centers — one in Massachusetts and one in West Virginia.
The gowns were missing the necessary holes for hands to slip through. A packing slip provided with the supplies includes a note with the logos of the Defense Logistics Agency, Centers for Medicare and Medicaid Services and Federal Resources, a distribution company, titled “Operation Commitment to Care.”
“Within this package you’ll find personal protective equipment necessary to provide safety for your staff and your patients,” the note reads.
Lori Mayer, spokesperson for the nursing home center, told CNN in a statement that despite the faulty gowns they were thankful for the PPE they’ve received from FEMA.
“While we are not specifically tracking FEMA shipments of the PPE at the center level, we can provide a few instances where we have had issues with the PPE received,” Mayer said.
She added: “We are not aware of other issues other than the reality that a one-week supply is obviously not enough given the complexity of the virus which continues to impact nursing homes.”
The American Health Care Association/National Center for Assisted Living, which represents more than 14,000 nursing homes and other long-term care facilities in the US, said facilities have received supplies, but agreed “these shipments will not be enough to ensure our facilities have an adequate amount of vital protective supplies in the months ahead.”
The Washington state official shared photos of a large blue tarp that was intended to serve as a gown and surgical masks designed with what appears to be paper, not elastic string, to wrap around the ears.
“Frankly, these supplies are unusable,” the official said. “They pose an infection risk and are not suitable for nursing homes or for any health care setting and we’re hearing significant concerns from the nursing homes that are receiving them about whether or not they can be used at all.”
In a letter to Vice President Mike Pence, dated June 10, Washington Gov. Jay Inslee urged the administration to do more to remedy persistent supply shortages, including using the Defense Production Act to ramp up manufacturing of equipment.
“Our current situation will only become more dire as more businesses reopen and more Americans head back to work — putting additional strain on a system that is already unable to meet demand,” Inslee writes. “States need the federal government to harness its power under the Defense Production Act and finally address the critical need for PPE, in much the same manner as it has done for ventilators and testing supplies.”
In late March, the Health and Human Services inspector general launched a review into nursing homes and their preparedness, acknowledging that long-term care facilities are “particularly vulnerable” to disease outbreaks.
The review is intended to determine whether facilities “that received Medicare or Medicaid funds complied with new Federal requirements for life safety and emergency and infectious disease control preparedness,” according to the HHS IG. The review is expected in the coming months.
The-CNN-Wire
™ & © 2020 Cable News Network, Inc., a WarnerMedia Company. All rights reserved.